Red light therapy science has gone from niche lab research to a mainstream wellness conversation. People are asking whether near infrared. This article distils decades of research, clear clinical evidence, practical uses, and realistic expectations so you can make an informed decision about photobiomodulation.
What is photobiomodulation? (red light therapy science explained)
Photobiomodulation, often shortened to PBM, is the medical name for what most call red light therapy. Put simply, it is the application of specific wavelengths of light to tissues to stimulate biological repair and reduce inflammation. Think of it as delivering a gentle, therapeutic signal that helps cells function better.
"It's called photobiomodulation. It's the registered name with the Natural Library of Medicine in America. And we call it PBM for short."
That short description hides a lot of nuance. The wavelengths used are typically in two bands: visible red light (around 630–660 nm) and near infrared light (around 800–850 nm). Those wavelengths penetrate tissues differently, with red light acting more at the skin and superficial tissues and near infrared reaching deeper muscles and sometimes nervous tissue.
Does it actually work? The evidence base for red light therapy science
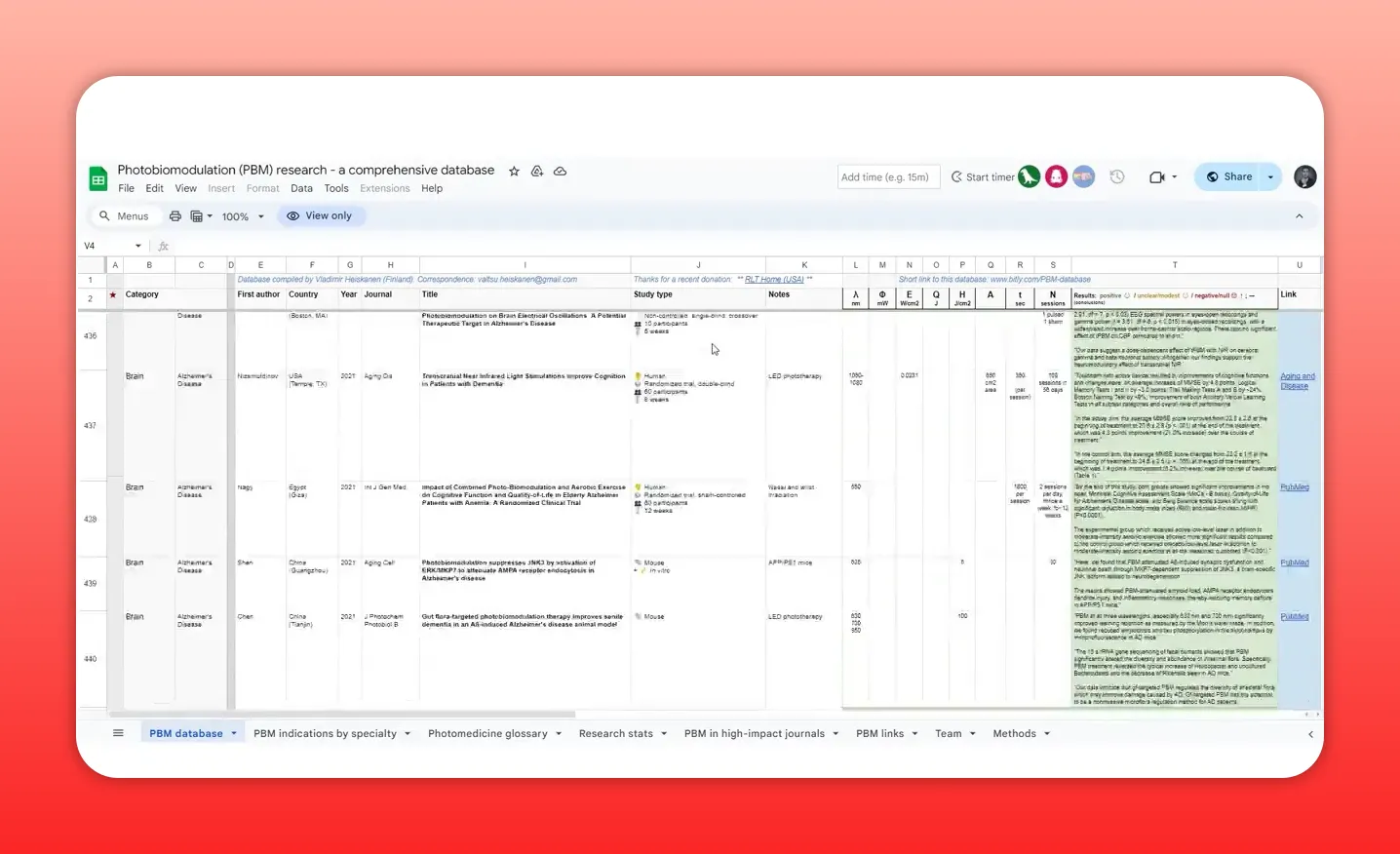
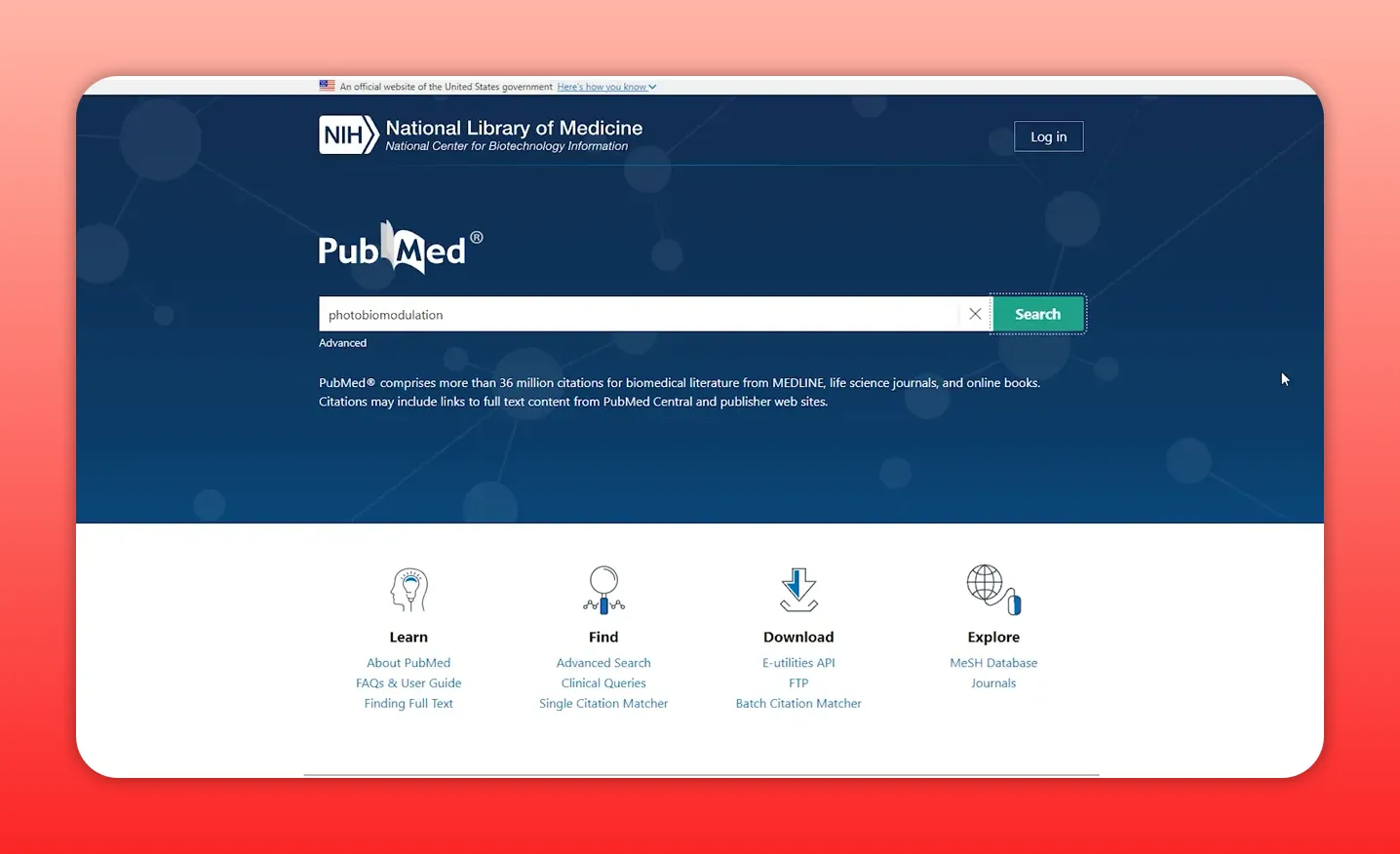
If you measure legitimacy by published research, photobiomodulation stacks up. There are thousands of peer-reviewed papers and many randomized, placebo-controlled clinical trials. The scientific literature includes studies on degenerative diseases, acute injuries, and specific clinical applications.
Key points about the evidence:
- There are thousands of publications investigating PBM and related mechanisms.
- More than a thousand randomized controlled trials support benefits across a range of conditions.
- Clinical use spans wound healing, pain reduction, osteoarthritis symptom relief, and neurological injuries among others.
That does not mean PBM is a miracle cure for everything. Rather, the cumulative red light therapy science points to consistent biological effects and promising therapeutic outcomes when protocols are matched to conditions.
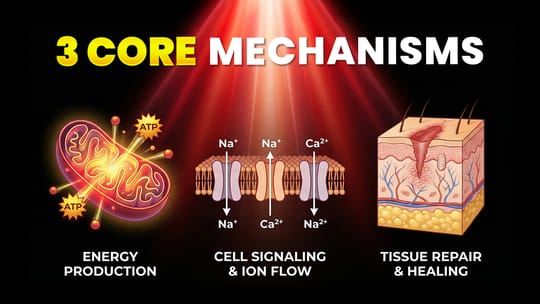
How it works: simple mechanisms behind complex biology
At the cellular level, photobiomodulation influences mitochondria, the tiny energy factories inside cells. When target wavelengths are absorbed, cellular respiration can become more efficient, often resulting in increased ATP production — the molecule cells use for energy. Improved mitochondrial function helps cells repair, replicate, and resist stress.
Other important mechanisms include:
- Reduced oxidative stress: PBM can lower the production of reactive oxygen species, commonly called free radicals, which are linked to inflammation and cellular aging.
- Anti-inflammatory signalling: Light can modulate cytokine responses and reduce chronic inflammatory signalling pathways.
- Improved microcirculation: PBM can increase local blood flow and support nutrient delivery and waste removal.
- Neuroprotective effects: In some studies, near infrared light supports neuronal survival and recovery after injury.
"If it only did one thing, it's really good at reducing the production of free radicals in the body and thereby also reducing inflammation."
Those mechanisms explain why PBM helps in places as different as wound beds, arthritic joints, and injured brain tissue. The underlying theme is enhanced cellular resilience and reduced chronic stress.
Clinical applications and real-world results
Medical practice and research have explored many uses. Here are examples where the evidence is strongest or growing rapidly:
- Wound healing and scar reduction: PBM accelerates tissue repair and is used in clinics for chronic wounds and post-surgical recovery.
- Pain management and musculoskeletal injuries: Studies show symptom relief for conditions such as tendonitis and osteoarthritis.
- Neurological injuries: Early trials and animal studies suggest benefits in traumatic brain injury and stroke recovery.
- Viral lesion support (e.g., cold sores): Clinical and anecdotal evidence indicate PBM can shorten herpes simplex outbreaks and reduce scarring.
- Skin and aesthetic uses: Although fewer large-scale trials exist, many users report improvements in skin tone and texture, driven by reduced inflammation and enhanced collagen activity.
One practical example involves cold sores. Many people find small handheld devices useful to treat herpes simplex lesions early in the outbreak, shortening the duration and limiting scarring. That outcome lines up with clinical reports and controlled studies.
Animal research and aging: what the lab studies tell us
Animal experiments provide insights humans cannot ethically receive. Studies in rodents show that regular PBM exposure can slow markers of neural aging and improve cognitive outcomes in models of degenerative disease. These results are encouraging and provide biological plausibility for human trials, but direct translation always requires clinical confirmation.
Safety and practical considerations for beginners
Safety is one reason PBM has become popular: when used as intended, red and near infrared light is non-ionizing and well tolerated. Typical side effects are minimal. Still, a few important safety notes:
- Eye protection: Avoid looking directly into high-intensity LEDs or lasers. Use proper goggles when recommended.
- Photosensitivity: Some medications increase light sensitivity; check with a healthcare professional if taking photosensitizing drugs.
- Dosage matters: Too little light produces no effect. Too much can reduce benefits. Match irradiance, wavelength, and treatment time to the condition.
- Device quality: Choose devices with published specifications and safety certifications. Clinical-grade equipment will have more reliable output and documentation.
Because protocols vary across studies, follow manufacturer guidance or clinical protocols, and consult a clinician for medical conditions.

Choosing a device: what to look for

The market now ranges from small handheld units to full-body panels. Here are the essentials to evaluate when comparing options:
- Wavelength: Look for panels or devices that clearly state the wavelengths used, typically 630–660 nm for red and 800–850 nm for near infrared.
- Irradiance (power density): Measured in milliwatts per square centimetre. Higher irradiance reduces treatment time but must be balanced to avoid overexposure.
- Energy delivered (fluence): Measured in joules per square centimetre. Many studies report therapeutic windows; check clinical literature for condition-specific guidance.
- Coverage area: Handhelds are great for targeted lesions; panels are better for systemic or larger-area treatments.
- Evidence and documentation: Prefer brands that provide links to published studies or independent testing.
Practical starter setup: a small, quality handheld for acute lesions (e.g., cold sores) and a medium-sized panel for muscle recovery or skin work is a sensible path for many people.
Protocols in brief: common clinical approaches
Exact protocols depend on the condition and device. Many trials and clinics use regular, repeated sessions rather than single treatments. General patterns include:
- Short sessions of a few minutes per treatment spot for handheld devices, repeated daily or several times per week.
- Panels used for 10–20 minutes per area, two to five times per week, depending on device power and target tissue depth.
- Consistent treatments over weeks produce cumulative benefits in most trials.
Because therapeutic windows vary, refer to credible clinical sources or product documentation for specific dosage recommendations.
Where to find reliable information and communities
Good information helps separate marketing from science. Use these resources to dig deeper into red light therapy science:
- PubMed: Search the database for "photobiomodulation" plus the condition of interest to find peer-reviewed studies.
- Specialist conferences: Scientific meetings on PBM gather researchers and clinicians who present the latest trials and mechanisms.
- Clinical manufacturers and academic collaborations: Some companies publish clinical trial results tied to their devices; look for independent studies too.
- Focused communities: Practitioner and user groups can be useful for practical tips, but always verify claims against peer-reviewed evidence.
Common myths and realistic expectations
Red light therapy science is robust in many areas, but expectations must be realistic:
- Not an instant fix: Unlike fictional depictions, PBM is not an instant heal. Benefits accumulate over repeated treatments.
- Not magic for appearance: While users often report skin improvements, the evidence for cosmetic effects is less extensive than for medical applications.
- Not a substitute for medical care: Use PBM as an adjunct in consult with healthcare providers for serious conditions.
How to get started with confidence
If you want to experiment responsibly:
- Define your goal: Are you targeting a cold sore, joint pain, skin tone, or general recovery? Different goals require different devices.
- Research the evidence: Search PubMed for "photobiomodulation" plus your condition to see what protocols researchers used.
- Choose a reputable device: Prefer devices with published output specs and any clinical data.
- Start conservatively: Follow manufacturer guidelines and increase exposure only if needed and safe.
- Track results: Keep a short log of sessions and outcomes to determine effectiveness for your situation.
Final thoughts on red light therapy science
Photobiomodulation is not a passing fad. The growing body of controlled clinical research and decades of mechanistic studies make the case that targeted light can be a powerful, low-risk tool in the therapeutic toolbox. It is most convincing in wound healing, pain relief, and certain neurological and inflammatory conditions. For cosmetic use and general wellness, the evidence is promising, though not as thoroughly funded as major disease research.
Explore clinical literature, choose devices with transparent specifications, and treat PBM as an evidence-based adjunct rather than a cure-all. With sensible expectations and consistent use, red light therapy science can be a meaningful addition to recovery, resilience, and everyday well-being.
Where to read more: start with peer-reviewed studies by searching "photobiomodulation" on PubMed, and consider attending specialised PBM conferences to hear the latest clinical data and practical protocols from researchers and clinicians.
Found This Interesting? Look At These Articles
🔴 The Red Light Therapy Facial Fat Loss Link: Myth Or Reality?
🔴 Does Red Light Therapy Help Scars? The Science
🔴 Red Light Therapy For Skin: Beauty Benefits, Potential Complications, And More
🔴 Psoriasis With Red Light Therapy: Potential Game-Changer?
Have You Seen These Reviews
🔴 Rouge G4 Pro Review: Most Advanced Red Light Panel Yet?
🔴 Best Red Light Panel Yet? Block Blue Light Mega Review
🔴 $800 Red Light Mask Has Lasers… But Why?
🔴 Omnilux Contour Mask Review: Still Worth It in 2025?
Alex's Bio
Alex Fergus wrote this blog post. Alex is an ISSN Sports Nutrition Specialist, Fitness Professional, and certified Superhuman Coach who continues to expand his knowledge base and help people worldwide with their health and wellness. Alex is recognized as the National Record Holder in Powerlifting and Indoor Rowing and has earned the title of the Australian National Natural Bodybuilding Champion. Having worked as a health coach and personal trainer for over a decade, Alex now researches all things health and wellness and shares his findings on this blog.